Multiple Sclerosis and Seating - What To Consider
It is a life-long condition generally diagnosed in 20’s – 30s and is around 3 times more prevalent in women than men.
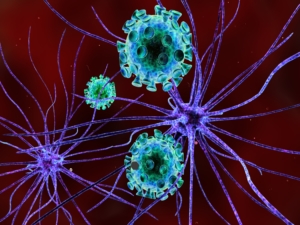
Multiple Sclerosis (MS) is an autoimmune condition that affects the brain and spinal cord. This essentially means that the body’s immune system tries to fight a healthy part of the body, in this case the myelin sheath that protects the nerves of the spinal cord and brain.
Signs and symptoms
- Fatigue.
- Reduced mobility.
- Visual problems.
- Urinary incontinence.
- Numbness or tingling.
- Muscle stiffness and spasms.
- Problems with balance and co-ordination.
- Information processing deficits.
However, depending on the type of MS the person has these symptoms vary in severity or presentation.
Types of MS
Relapse Remittance MS
8 out of 10 people diagnosed with MS have a relapse remittance type. This means that they have flare ups (or relapses) which result in new or recurring symptoms at various and often unpredictable times in their life. The symptoms get progressively worse over a period of days, weeks or months but then recover over a similar period. The symptoms may disappear completely or persist at a lower level leaving the person slightly less functioning than they had been pre-relapse.
Over a period of decades some people with RRMS develop Secondary Progressive MS.
Secondary Progressive MS
This means that symptoms gradually worsen over a period of time without an obvious episode of relapse.
Primary Progressive MS
Only 1 in 10 of people diagnosed with MS have a progressive worsening of the condition. The primary therefore refers to it being the first part of the disorder rather than having developed from RRMS.
Considerations when looking for a suitable chair:
Considering seating for someone with MS should not focus on the MS itself given the significant variances in presentation, but more on the person’s goals, lifestyle, health promotion and specific symptoms. Therefore, basic assessment principles apply:
- The height of the seat must allow the user to sit with their feet flat on the floor. Always remember to ask whether a client uses slippers or not as this will affect height.
- The seat width needs to provide enough support to prevent a user slumping to either side in the chair.
- The seat depth should be long enough to support the femur, but not too long to cause pressure problems behind the knees.
- The armrest should be at a suitable height that supports a neutral resting position with no shoulder or shoulder girdle elevation. However, the height should consider the ergonomics of a stand and therefore create enough of an angle to support the upper limb push into standing.
- A motor mechanism that supports rising can facilitate a safe transition from sitting to standing whilst also providing a physical prompt to initiate movement and therefore reducing fall risks.
- The handset should be one that the user can operate without any pain or discomfort.
- The back should be high enough to support the upper limbs and avoid pressure points on the large joints.
- The fabrics and any comfort padding should be discussed with the client to make sure it meets their needs.
- Always set goals with the client/carer and ensure that the recommended chair will achieve them.
In addition to these standard principles you should consider the person’s presentation when they have a relapse or indeed their likely progression based on diagnosis of type. For example, some people with MS can become extremely fatigued at certain times of the day or indeed season (as MS symptoms can be affected by temperature extremes) so you need to think about whether the chair needs to allow for rest throughout the day and manage exercise tolerance.
Recommended seating
Below we have linked to some of the chairs in the Repose range that might be considered, but their suitability will depend on the progression of the conditions. Others in the range may be suitable, but this will again depend on the clients conditions.
